Insulin 101: What It Does, Why It Matters, and How to Improve Sensitivity
Insulin 101: The Hormone That Makes (or Breaks) Metabolic Health
By Dr. Lisha Town
Insulin isn’t “good” or “bad.” It’s a powerful signal your body uses to store and use energy. In this post, you’ll learn what insulin does, how insulin resistance develops, which labs actually matter, and the simplest ways to improve insulin sensitivity.
What insulin actually does
- Clears glucose into muscle and liver after meals
- Stores extra energy as glycogen (and as fat when stores are full)
- Pauses fat-burning temporarily (insulin suppresses lipolysis)
- Supports building and repair (protein synthesis)
Goal: Let insulin rise after you eat - and fall between meals.
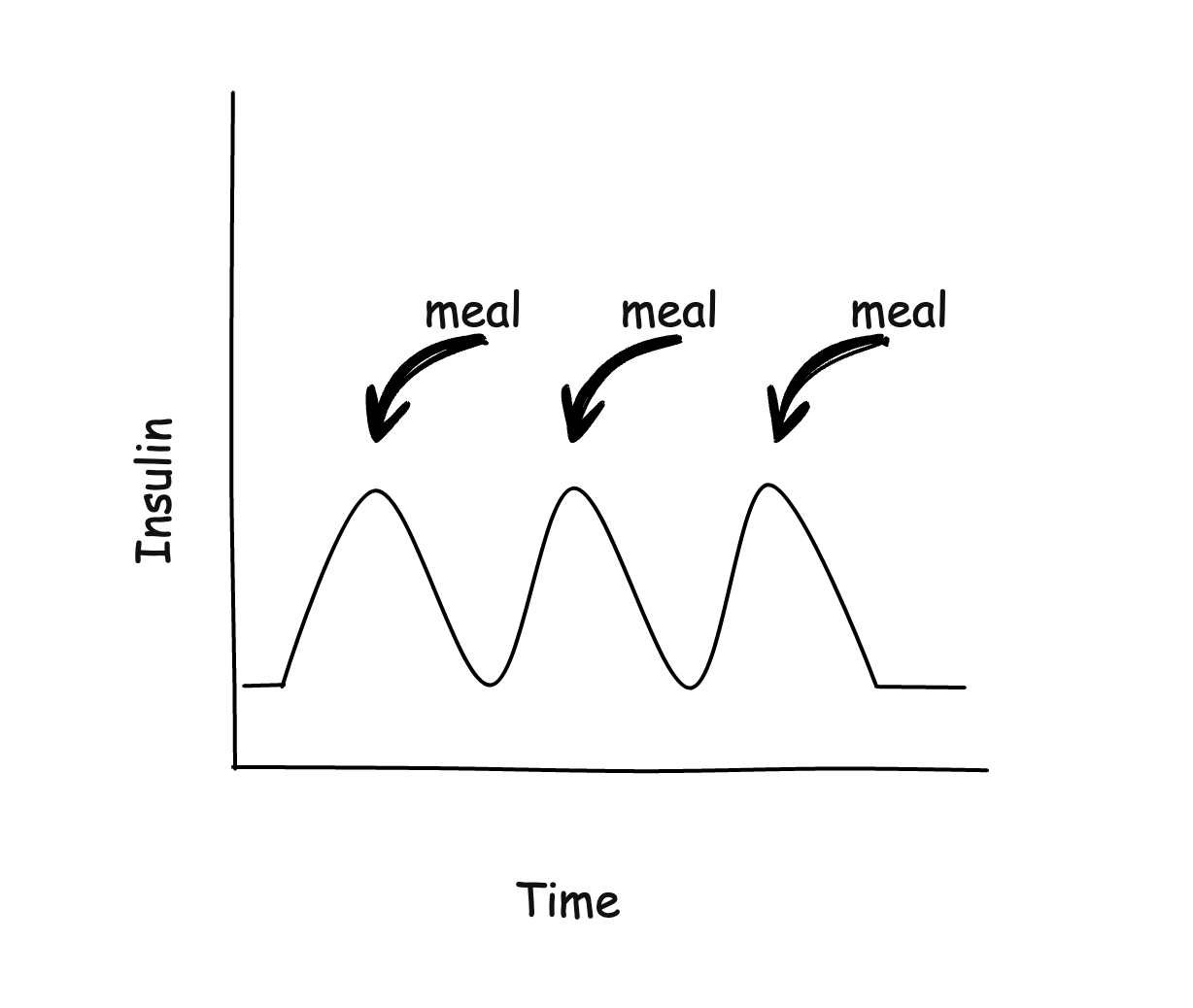
The healthy daily rhythm
- After meals: insulin rises, glucose moves into cells, then both drift down within a couple of hours.
- Overnight: insulin should be low; a small morning bump (the “dawn phenomenon”) can be normal.
- Aim for: meal-timed rises with low valleys between meals and overnight.
What is insulin resistance?
Insulin resistance (IR) means your cells don’t “hear” insulin well, so the pancreas “shouts” louder. Have you ever been around kids you are just constantly trying to get your attention? Eventually, you just start tuning them out. In this example the 'parent' is the cells and the 'kids' are insulin. Too much exposure means your cells start to tune it out.

Over time, higher insulin + higher glucose can lead to:
- Visceral (waistline) fat gain
- Higher triglycerides and lower HDL
- Inflammation and vascular stress
- PCOS symptoms in many women
- Prediabetes → type 2 diabetes if unaddressed
Why IR happens: ultra-processed food patterns, inactivity, poor sleep, chronic stress, and fat stored in the liver/muscle (ectopic fat) all play roles.
Numbers to know (use with your clinician)
• Fasting insulin: many metabolically healthy adults ~2–6 µIU/mL
• HOMA-IR = (fasting insulin × fasting glucose)/405 → lower is better (≤1.0 is often insulin-sensitive; ≥2.0–2.5 suggests IR)
• TG/HDL ratio (mg/dL): <1 favorable; >2 suggests IR risk
• Waist: <35" (women), <40" (men); lower is better for height
• Post-meal glucose:keep the peaks <140 mg/dL and return to baseline within 2-3 hours
(Coaching targets, not diagnoses - interpret in context.)
Five common myths
- “It’s only calories.” Energy balance matters, but food quality changes hormones and fullness.
- “Carbs are evil.” Quality and context matter. Many do well with fiber-rich, minimally processed carbs - especially when followed by a short walk.
- “Protein spikes insulin like sugar.” Protein causes a modest rise in insulin and also raises glucagon; net effect usually supports stability and lean mass.
- “You must do extended fasts to fix insulin resistance.” Fasting is one tool. Many succeed with meal structure, food quality, walking, sleep, and strength training.
- “Fruit always ruins glucose.” Whole fruits, especially berries - when eaten in moderation - cause only a modest rise (if you are insulin sensitive).
How to improve insulin sensitivity
1) Eat for stable insulin
- Lead with protein + produce
- Carb order: protein/veg first, starch last (if you have a starch at all)
- Eliminate ultra-processed foods
- Meal timing: 2–3 satisfying meals; avoid constant grazing
- Smart extras: 10–15 min walk after meals; splash of vinegar may help some people
2) Move like you mean it
- After-meal walks: 10–15 minutes
- Strength training: 2–3×/week (muscle = glucose can be absorbed by the muscles independent of glucose)
- 1–2 HIIT sessions when recovered - sprinting is a great option
- Extras: stand, stroll, take stairs
3) Sleep like it’s medicine
- 7–9 hours with a fixed wake time
- Dim lights/screens 60–90 min before bed
- Morning outdoor light for 5–10 minutes
4) Down-shift daily stress
- Paced breathing: 5 min @ ~6 breaths/min
- Mindfulness or prayer: 5–10 min
- Nature & social connection each week
5) Medications (talk to your doctor)
Insulin-sensitizing meds can help select patients. If you use insulin/secretagogues, changing diet/exercise may require dose adjustments - coordinate with your clinician.
A simple 14-day reset
- Daily: Protein-anchored meals • 10–15 min walk after a meal • 5 min breathing • Morning light
- 3×/week: 30–45 min brisk walk or cycle
- 2–3×/week: Full-body strength, 20–30 min
- Always on: Water first • Eliminate ultra-processed foods • Consistent sleep/wake
FAQ
Is the “dawn phenomenon” bad?
Not necessarily. Mild morning elevations are common. Focus on overall patterns and A1c/CGM trends.
Do I have to cut all carbs?
No. Many thrive with protein-anchored meals, fiber, and strategic carbs, while avoiding ultra-processed foods.
What about women & midlife?
Perimenopause/menopause can increase IR risk. Protein, strength training, sleep, and stress care are foundational.
Can insulin be too low?
You want responsive insulin - rises with meals, low between. Chronically suppressed insulin isn’t the goal.